Abstract
An immediate implant placement procedure is when an implant is placed at the same time as the natural tooth is extracted. The procedure enables shortening of the healing process, as there is healing at the extraction site and implant insertion at the same time. A viable solution for both the dentist and the patient, as the procedure can be performed in a single visit to the clinic, immediate implant placement is most common when tooth extraction is due to trauma, endodontic lesion, root fracture, root resorption, root perforation, unfavorable crown to root ratio, and when bony walls of alveolus are still intact.

To enable successful immediate implant placement, it’s vitally important to select an implant that’s best suited for each individual case. Let’s take a look at the clinical aspects, the differences between various implant families, and our recommendation of which implant to use in every clinical case.
Are all implants really the same?
Dental implants may yield almost similar clinical success rates, however, there are notable differences in using them, and as such, their suitability for different clinical cases.
Dental implants can be divided into two key families:
- Active implants – Achieve a very high primary stability and serve more complex clinical cases
- Passive implants – These implants are gentler with the bone, are generally more conservative, and are intended for use in simpler clinical cases
Be it a passive or active implant, it’s important to ensure that the implant deliver exceptionally high primary stability and reduced bone pressure, in order to preserve the bone for the long term.
The relationship between the bone and the implant
To best understand implant quality and long-term durability, and the requirements for each clinical case, we must first understand the relationship between the bone and the implant. When an implant is placed, it usually exerts high pressure in the cortical area. This area consists of type 1 bone, which also suffers from impaired recovery due to low blood supply. Therefore, when an implant is placed in cortical bone, it can cause a lot of damage that would be difficult to repair. However, the implant gains most of its primary stability from this area.

In contrast, the apical zone generally consists of spongy bone with a lot of marrow spaces. This means that the blood supply to this area is very good, and that the recovery of this area is better, as well as its ability to absorb the pressure. However, in this scenario, the implant gains the least of its primary stability from this area.
To facilitate a successful procedure, we want to select an implant that can achieve very high permeability from the apical area of the bone, while reducing the pressure in the cortical area. This way, we will not lose valuable bone, and we will prevent bone resorption in the first year after implant placement, and for the long term.
In recent years, the world of implantology has changed dramatically with the advent of advanced implant design and manufacturing processes. Today, most clinical cases are performed with immediate implantation, which raises the question of where the implant gains its primary stability from. When the implant is placed in an extraction socket, all the primary stability of the implant is derived from the apical area of the socket. Therefore, when it comes time to selecting the type of implant for immediate placement, it’s essential to think of the apical part of the implant as the most important segment for immediate primary stability.
The dental implant: What are its parts?
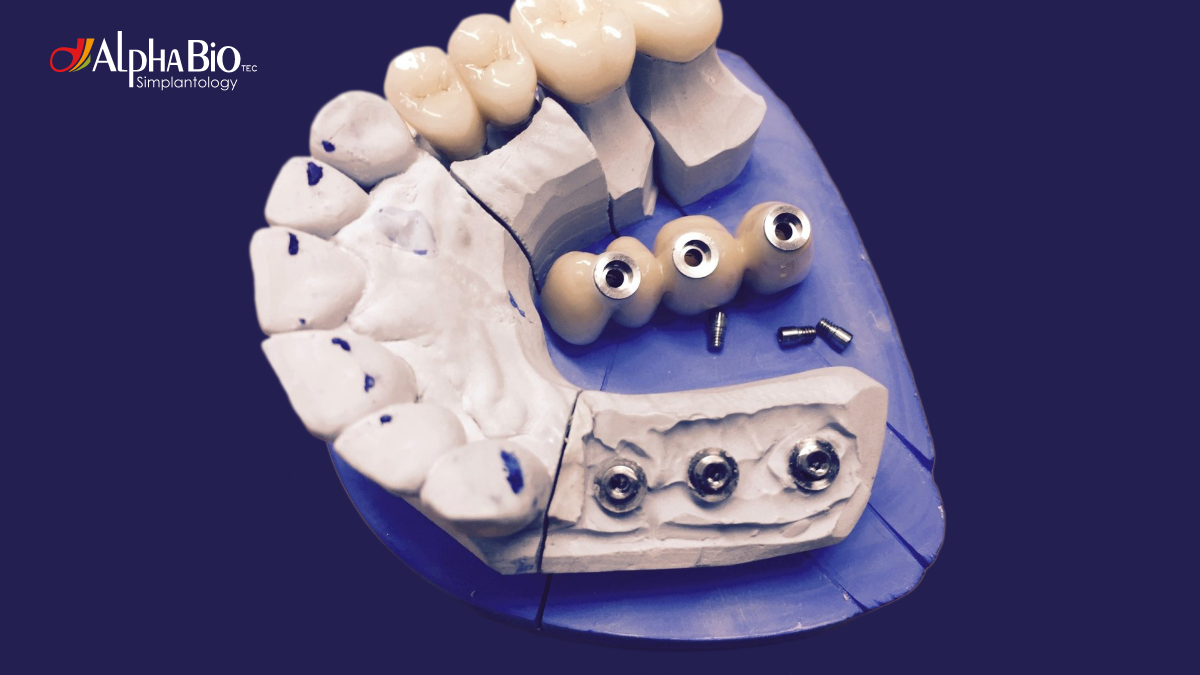
In the simplest sense, dental implants are composed of several different parts, each of which has a specific function in the immediate placement procedure, to support bone preservation, primary stability, and the healing process.
Coronal part – Essential for bone preservation, as by reducing bone pressure, we can preserve the bone for the short and long term. The implant gains most of its primary stability from the coronal part, and it is generally the widest area of the implant design.
The head of the implant can be back-tapered or straight, machined, micro-threaded or completely smooth, with the option to enable platform switching between the implant and the abutment. Usually, the coronal part does not contain active threads or micro-threads, and cannot drill itself through the bone, therefore, using implants with threads in its coronal part, may enable the implant to cut through the bone, and reduce pressure.
Body/core – Responsible for the implant's primary stability. The shape of the body or core can be very cylindrical, straight or tapered, or it can be combined – meaning that part of the body will be straight, and part will be tapered. A cylindrical body means that the implant condenses the bone laterally when it penetrates deeper into the area.
Threads – Responsible for the fundamental character of the implant, and whether it would be active or passive. Threads are vitally important for the implant’s cutting efficiency, and for the dentist's ability to feel when the implant is successfully placed into the bone.
Apical part – The most important part for primary stability in immediate implantation. The apical part is the primary part of the implant that cuts all the way through the bone, and directs the implant into the bone, and as such, it should be as narrow as possible. To facilitate higher primary stability, we must drill less, and then place the implant into the bone as it cuts its way in. The threads in the apical area should be very deep, so that it will be able to penetrate hardly into the bone, and gain more primary stability in the apical area.
Which implant to use in each clinical case?
When deciding on the most suitable implant for each individual case, an active implant would be a trusted and reliable universal choice that can serve all of your clinical cases and patient needs. For simple clinical cases, a conventional cylindrical implant is sufficient, however, it should not be used in complex implant placement procedures.
Successful immediate implantation: What implant to choose?
In immediate implantation, the bone bed preparation is not standard, as most of the drilling takes place in the apical part of the socket. The wall is usually angled, and in many cases, the implant slips when attempting to place it into socket. Therefore, an implant with a centering feature in its apical part would be recommended to center the implant at the exact location of the osteotomy, and slide easily into narrow hole. Remember, that the apical part of the implant should be narrow enough to fit in the osteotomy.

The implant's core should be firm to promise stability and primary engagement with the bone. It should be slightly tapered all the way down, to condense bone as it advances apically, and provide stability even in type III and IV bone.
The implant's threads should be very active, with high cutting efficiency to enable smooth cutting through the bone. The active, wide implant threads would also provide high primary stability. A lead of 2.4mm between the threads enables the creation of deeper threads, that become even deeper towards the apical part with the narrowing of the implant core. The threads in the apical part are the first to engage the osteotomy, and therefore, should have robust cutting ability, while in the middle part of the implant, we would use wider threads, with bone condensing properties.
Making the right choice and the "best" choice
Active dental implants serve us well in immediate implantations, and closed and open sinus lifts, facilitating smooth and easy insertion into the bone, and enabling high bone condensing ability. To effectively support immediate implant placement, it’s important to first understand your clinical case, and determine whether the immediate implantation procedure will be simple or complex. Based on your assessment, decide on what implant would best enable bone preservation, primary stability, and the healing process. Keep in mind that in most clinical cases, an active implant is a good universal choice, to serve both your needs, and the long-term needs of your patient.
It’s equally important to choose an implant that is easy to learn, and simple to use – a single interface supported by a single surgical kit will provide the best possible solution for most clinical cases.
As immediate implant placement continues to evolve at a rapid pace, it’s fast becoming the solution of choice for dental clinicians worldwide. With fewer surgical interventions, lower overall treatment time, reduced soft and hard tissue loss, and psychological satisfaction to the patient, immediate implant placement with the right implant for each individual clinical case, will continue to serve both dentists and their patients for many years to come.
Related Blogs
Immediacy | Grafting & Biomaterials

Post-Implant Removal with Bone Regeneration And Immediate Loading Using Alpha-Bio Tec's MultiNeO™ implant
Guided Surgery | Digital Dentistry | Tips & Techniques

Guided Implant Surgery: A Step up from traditional solutions – What you need to know
Education | Tips & Techniques

What do you need to know before you start - Implant Placement
Immediacy | Tips & Techniques

7 Advantages of Immediate Tooth Implantation
Education | Overdentures | Tips & Techniques
Getting Started with Implant Prosthetics: What you need to know
Guided Surgery | Digital Dentistry | Immediacy


