Growing in popularity, advanced dental implant surgery, or "implantology," is a procedure that replaces missing teeth with artificial ones that effectively look and perform like real teeth. Today, implant surgery is a viable option, and a welcome alternative for patients whose only choice was either dentures or bridgework.
Dental implants are a commonly used treatment option for a variety of restorative cases. They can be used for replacement of any number of teeth, from a single tooth, to a full dental arch, to restore the masticatory and phonetic function of the patient, and their aesthetic appearance. Dental implants can also be used as retentive elements for removable prostheses, improving stability, and enhancing the patients' day-to-day comfort, not to mention, confidence.
Let's take a closer look at the "must-haves" – the essential stages of implant surgery.
Determining the Number of Implants and their Distribution
The number of implants to be placed depends on the number of teeth to be replaced, the type of prosthetic system to be used, and bone availability. It's believed that the ideal number of implants to be placed is equal to the number of missing teeth, however, in many cases, reaching the ideal is impossible, as it's determined by the patient's condition.

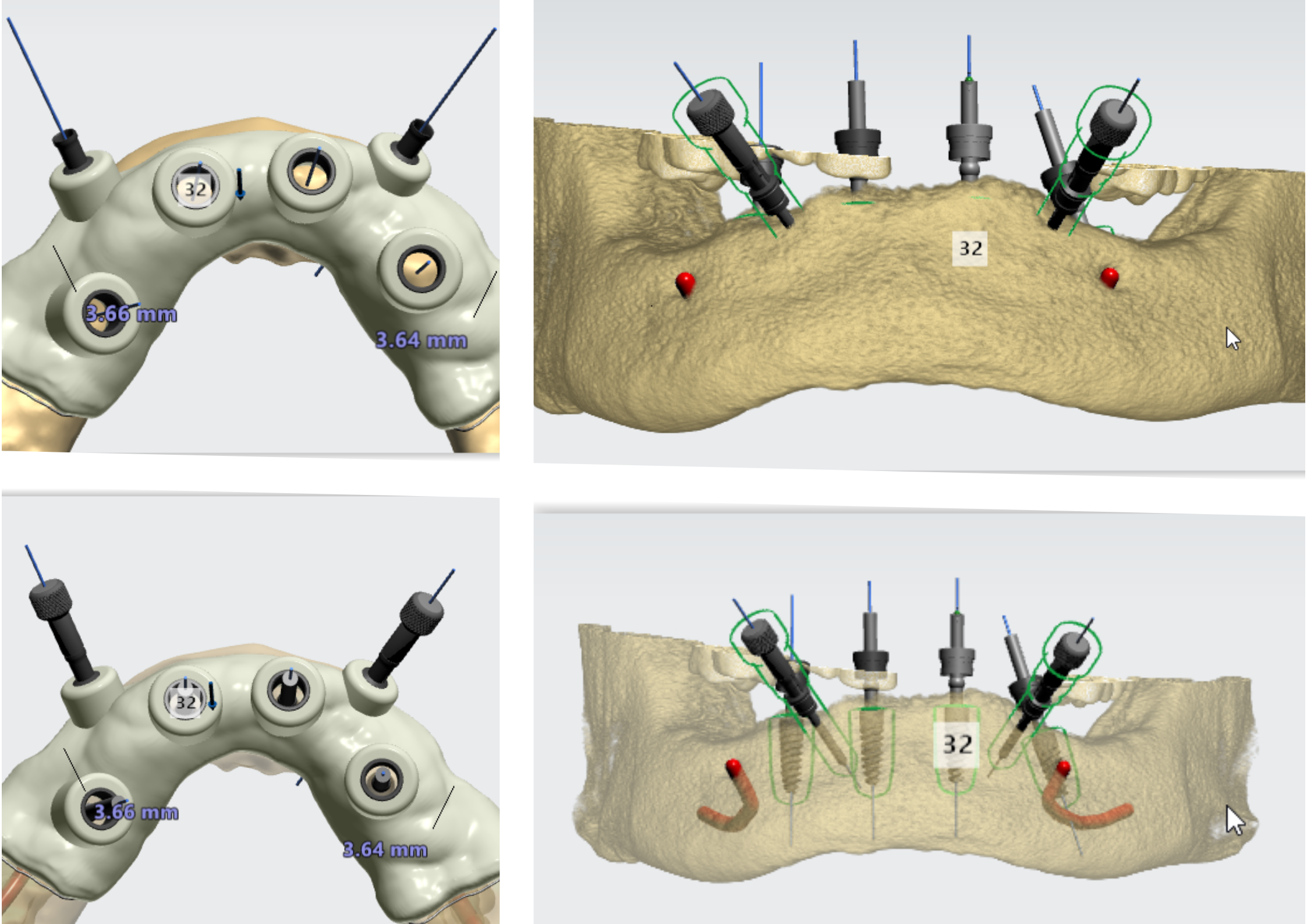
As such, the minimum number of implants to be placed in one jaw is determined by 2, and adding 1. For example, if 6 teeth are to be replaced, the ideal number of implants is 6. The minimum number of implants is 6/2+1 = 4 implants. When distributing implants, there must be 1.5-2mm of bone between a tooth and the edge of an implant, and 3mm between two implants.
Determining Implant Diameter and Length
When placed in the bone, the implants should have sufficient bone support on all sides. It's important to maintain at least 1.5mm of bone thickness on the buccal and lingual sides of the implant, and a safety margin from adjacent anatomical structures (e.g. the maxillary sinus or the inferior alveolar nerve canal). By determining the width and height of the alveolar crest, you'll be able to choose an implant with the right diameter and length. Implant length selection is also determined by the planned level of the implant placement – supracrestal (common for tissue level implants), juxtacrestal, or subcrestal (submerged).
Making an Incision and Reflecting a Flap
When an incision is made to place an implant, the scalpel must be positioned at 45° and inserted until bone is touched (full thickness incision). If there are teeth adjacent to both sides of the incision area, it's best to perform a mid-crestal incision followed by an intra-crevicular incision. If teeth are only adjacent on one side of the incision area, a mid-crestal incision should be made 15-20mm beyond the placement of the last implant, followed by an intra-crevicular incision at the adjacent tooth.
In edentulous patients, a mid-crestal incision should be made up to 15 20mm beyond the placement of the last implant, followed by a vestibular release in the central area, to ensure flap movement. After the incision is done, you can use a curette or periosteal elevator to reflect it, and expose the bone bed.
Flap-less and Post-Extraction Implant Surgery
In some cases, it's not necessary to make incisions or flaps, for example, when implants are placed immediately post-extraction, into the extraction socket. This is an atraumatic and minimally-invasive technique, geared towards preserving the natural bone structures. However, if the buccal bone plate is broken or missing, GBR (Guided Bone Regeneration) is required adjacent to the immediate implant placement.
Flap-less surgery can also be used in other implant placement cases, and is best performed in areas where bone thickness exceeds 7mm. It's beneficial for the patient, as it helps reduce the post-surgical trauma. However, working in a closed field without direct vision of the bone bed can increase the likelihood of mistakes during implant placement. Therefore, it's best to perform flap-less implant placement with a surgical guide, which would in turn, help minimize mistakes.
Drilling and Implant Placement
When placing the implant, use the manufacturer-recommended drilling protocol and tools to prepare the implant bed. The drilling protocol may differ between various implant types and bone quality (e.g. cortical bone vs. trabecular bone). After the drilling is complete, place the implant using a manual tool or a physiodyspenser.

It's important to determine the initial stability of the implant by measuring the force applied to place the implant. This can be done by using a torquemeter. Torquemeters are used to screw the implant into the bone tissue, as well as to precisely tighten the prosthetic components to an already integrated implant, while measuring the force applied (in Ncm). When the necessary force has been attained, the torque wrench snaps. Some dental professionals mistake torque ratchets for torquemeters, however, torque ratchets don't provide the exact Ncm value applied in the process, while torquemeters do.
The ideal torque value is 35 Ncm. This is also the minimum torque value indicated for immediate implants, or implants that would undergo immediate loading. Ideally, primary anchorage should be 40-45 Ncm. In general, the maximum torque value when placing the implant should not be greater than 45 Ncm. In submerged implants, a minimum torque value of 20 Ncm should be used. In cases of excessive friction when placing the implant, the implant should be removed. You should then apply the next drill size up to half of its length, and then attempt to place the implant again.
Summary
There are numerous advantages and benefits of dental implant surgery, namely that dental implants look and behave like a natural tooth, can effectively prevent bone loss, and they support the facial structure, with visually appealing results. What's more, implants are long-lasting, and don't limit what a patient can eat. Finally, for both the clinician and the patient, dental implants are cost-effective, when compared to other restorations that may require replacements on a regular basis.
Related Blogs
Education | Clinical Case

Education at the Heart of Alpha-Bio Tec. - Our 2026 Vision
Education | Webinar on-demand



.jpeg)